Are you tired of feeling lost in the world of medical billing? Do terms like “EOB” and “ICD-10” make you want to run for the hills? Well, fear not! This beginner’s guide to medical billing language is here to help you navigate the murky waters of healthcare.

Learning new terms about different fields isn’t just fun, it also broadens one’s wisdom and causes one to be more diligent. Roy Leslie Bennett, a Zimbabwean politician and member of the British South Africa Police writes in his book “The Light in the Heart” that: “No matter how much experience you have, there’s always something new you can learn and room for improvement.” The key to staying on top of one’s game is to never limit oneself to one field and to keep learning new things all the time.
Let’s start with the basics. Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for medical services rendered. The language used in this field can be confusing, so let’s break it down.
- HCPCS
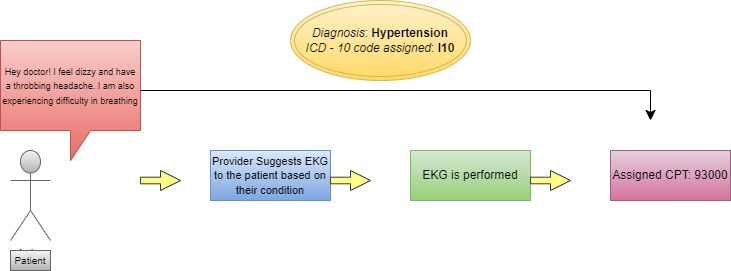
HCPCS stands for Healthcare Common Procedure Coding System. It is a standardized coding system used in the United States to describe and identify medical procedures, supplies, and services provided by healthcare professionals. HCPCS codes are used for billing, reimbursement, and statistical purposes.
The system consists of two levels:
Level I codes are based on Current Procedural Terminology (CPT) codes, which primarily describe physician services.
Level II codes are alphanumeric and cover a broader range of healthcare services, such as durable medical equipment, prosthetics, orthotics, and supplies.
Things you need to know about CPT:
- CPT is a five digit code
- It can be Numeric – Level I (70010 – Diagnostic Radiology Procedures of the Head and Neck ) or Alphanumeric – Level II (J0696 – Injection, ceftriaxone sodium, per 250 mg )
- ICD – 10
Moving on to the ICD-10 code. ICD stands for International Classification of Diseases and ICD-10 indicates its 10th volume. These codes are used to describe medical diagnoses and conditions. They help healthcare providers get paid for the right services based on the patient’s medical needs.
Things you need to know about ICD-10:
- According to latest revision of ICD, diagnosis codes (dx codes) always start with Alpha letters and end with numerics (Z23 – Encounter for immunization)
- ICD-10 codes can be 3 to 7 characters long
- Provider
In medical billing, the term “provider” refers to a healthcare professional or facility that provides medical services to patients. This can include doctors, nurses, hospitals, clinics, and other healthcare providers. Provider is also known as one of the three “Ps” of the healthcare industry.
- Claim
In medical billing, a “claim” refers to a request for payment for healthcare services that have been provided to a patient. When a patient receives medical services from a healthcare provider, such as a doctor’s visit or a surgical procedure, the provider submits a claim to the patient’s insurance company for reimbursement.

- Clearing House
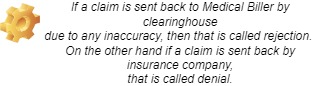
Now that you have a claim ready including all the information of the patient’s visit to the provider including patient information, insurance/payer information, CPT codes along with corresponding diagnosis code. Where does the claim go from here?
Now the claim has to go through a filtration process to make sure that they are properly formatted and contain accurate information before they are submitted to insurance companies. They can also help to identify errors or discrepancies in claims and work with providers to correct them before they are submitted for payment. This filtration is performed by a clearinghouse.
- Payer
Next we have the second P of the healthcare industry that is “Payer”. In medical billing, the term “payer” refers to an entity that pays for medical services on behalf of the patient. This can include insurance companies, government programs such as Medicare and Medicaid, and in some cases patients themselves if they are self-pay.
Moving on to some terminologies that can be a little tricky to figure out, but aren’t as complex as they seem.
- EOB
Now we have EOB. EOB stands for Explanation of Benefits. This document explains how much you owe for medical services and what your insurance company paid. It’s like getting a receipt, but instead of buying a new shirt, you’re paying for a visit to the doctor.
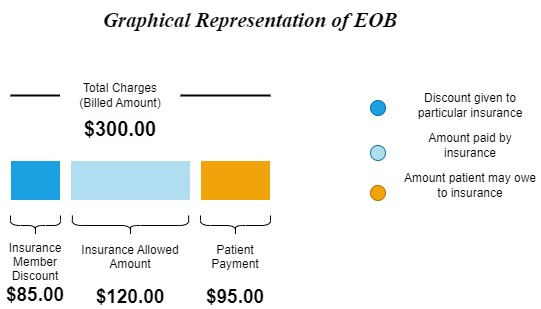
- Co-insurance
When you go to the doctor or hospital, your insurance helps pay for some of the costs. Co-insurance is the part of the cost you have to pay yourself, even after your insurance has paid their part. It’s usually a percentage of the total cost of the medical service or procedure, and the amount you have to pay can be different depending on your insurance plan. It’s basically the difference between the insurance allowable amount and the payable amount.
- Co-Pay
In medical billing, a “co-pay” or “copayment” is a fixed amount of money that a patient is required to pay out of pocket for a particular medical service or prescription medication. Co-pays are usually determined by the patient’s health insurance plan, and the amount of the copay can vary depending on the type of service or medication being provided.
- Deductible
The deductible is the amount that a patient must pay for healthcare services before their insurance plan begins to cover them. Deductibles are usually determined by the patient’s insurance plan, and they can vary in amount depending on the plan.
For example, if a patient has a health insurance plan with a $500 deductible, they would be required to pay the first $500 of their healthcare expenses out of their own pocket before their insurance plan would begin to cover the costs. A portion or all of the remaining healthcare expenses would be covered by the insurance plan once the deductible is met, depending on the plan.

I hope this short introduction to most commonly used medical billing terms will give you a sense of belonging in the respective field. Here’s to keep learning and thriving together!

